Management of Patellofemoral Pain
– information for clinicians
The information contained on this website is based on a high-quality living systematic review with network meta-analysis. An international team completed a large review on the evidence on the most effective treatment for patellofemoral pain. It took > 2 years to complete and was funded by TRYG-fonden (grant ID 118547).
The findings of the project have been published in the British Journal of Sports Medicine – and are available as open access: link to article. The systematic review (and this website) will be updated annually in the period between 2020 and December 2025 by the Center for General Practice at Aalborg University. If you are interested in keeping the review up to date, please contact Prof. Michael Skovdal Rathleff at misr@hst.aau.dk.
In the text below you will find a short description about the key methods (further details can be found in the published manuscript), the results of the study, and then the implications for practical management of patellofemoral pain. The last section includes practical details on the management of patellofemoral pain. These should serve as an indication of what can be done in practice. Management should always be tailored to the individual patient. This information is intended for use by healthcare practitioners.
Brief description of the study
Objective
To investigate the comparative effectiveness of all treatments for patellofemoral pain (PFP).
Methods
We conducted a Living systematic review with network meta-analysis (NMA) and ran a sensitive search in seven databases, three grey literature resources and four trial registers. We included randomised controlled trials evaluating any treatment for PFP with outcomes ‘any improvement’ based on a global rating of change scale, and pain intensity. Two reviewers independently extracted data and assessed risk of bias with Risk of Bias Tool V.2. We used Grading of Recommendations, Assessment, Development and Evaluation to appraise the strength of the evidence.
Results
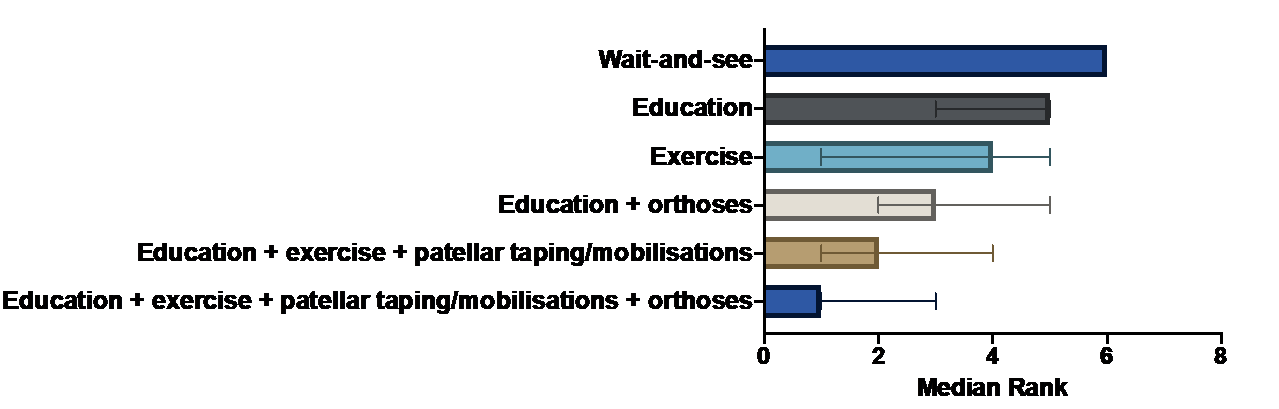
Twenty-two trials (with 48 treatment arms) were included, of which approximately 10 (45%) were at high risk of bias for the primary outcome. Most comparisons had a low to very low strength of the evidence. All treatments were better than wait and see for any improvement at 3 months. Education+exercise+patellar taping/mobilisations, with or without orthosis were superior to education alone. At 12 months, education or education+any combination yielded similar improvement rates.
The image below shows the ranking of the treatment most likely to be beneficial after 3 months. The lower the value, the more likely it is to be beneficial. The error bars indicate the 95% credible interval which underline that there is some uncertainty in our findings.
Implications for management of patellofemoral pain
Guidelines for musculoskeletal pain often recommend a wait-and-see approach. Based on this NMA, wait-and-see is the least effective treatment available for short term outcomes. Clinicians should therefore avoid a wait and see approach. You can consider a minimum of patient education at the first consultation and potentially add exercise, orthoses or patellar taping/mobilisations if the patient and you agree on the time requirements, cost and benefit. There was no evidence that one form of exercise was superior to another form of exercise, and patient preferences may be used to guide exercise selection. See concrete examples of hip and knee exercises and patient education in the bottom of this page.
Practical details on patient education, exercises, orthotics and patellar taping
As there is no golden standard proven to be more effective than another approach, we have listed some commonly used options that are easily accessible and commonly used in the trials included in the NMA.
Patient education
Education can be delivered in both one-to-one-sessions with a health-care practitioner or delivered in a leaflet/webpage, or as a combination. Current evidence suggest that education delivered through a health-care practitioner may be more effective than only giving patients a leaflet (ref) Education should be tailored to the context of your patient but typically it would include: information about PFP, information on pain and guidance on how to manage activity in the context of pain, without stopping all exercise. For further ideas on content, and how to deliver to your patients we have linked to two leaflets which provide this information for the patient (link to PFP leaflet for kids in English: LINK and Danish: LINK and adults with PFP in English: LINK and in Danish: LINK .
Exercises
Most studied exercise therapy routines have used a combination of supervised and non-supervised exercises. Pending the patients previous experience with exercises, it may be useful to refer the patient for an instruction on how to perform the exercises. In general, a relevant starting point could be an instruction for exercises targeting the knee and hip muscles, which can be performed unsupervised at home. The general aim would be to exercise 2-3 times per week and use 2-3 different exercises that are each repeated 3 times (i.e. 3 sets of each exercise) with 10-12 repetitions. The exercises should be done adequately heavy, so your patient feels fatigued towards the end of each set. It is completely fine to feel a bit of pain or discomfort around the knee when performing the exercises as long as it does not flair up afterwards or is markedly worse the next morning. In this case, you should ask your patient to reduce the load during each exercises or cut back 1 set of exercises (see previous links for exercise instructions).
Orthotics
The majority of studies of orthoses used prefabricated orthoses that allowed for some modifications to allow the physiotherapist to optimise the comfort fit for the patient. Apart from different sizes (e.g., length, volume) and the ability to trim the device to fit the patient’s shoe – improved comfort was enabled through different volume and hardness of devices that could be modified through heat moulding and/or addition of wedge. This is described in detail here.
Patellar taping
Sometimes patellar taping can be useful in addition to education and exercise. Several different taping techniques exist and it should be your patient's immediate response that help guide the type of taping. It is recommended to see a health-care practitioner to help find out which taping may be useful for your patient and teach them to apply it themselves. This video demonstrate some of the concepts and may be helpful for your patient to understand why taping can be useful: link to video.
Last update: November 2020

